Dentin hypersensitivity (DHS) is one of the most common complaints patients have, but often while in dental school, the focus is on the restorative needs of school clinic patients and DHS may be overlooked.
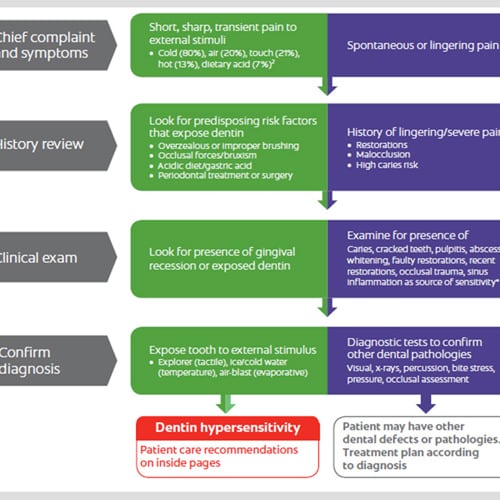
DHS has been defined as a short, sharp pain that is a response to non-noxious stimuli such as heat, touch, osmotic pressure, chemicals, or evaporative stimuli on exposed dentin that has open dentinal tubules. A diagnosis of DHS is a diagnosis by exclusion meaning that the short, sharp pain experienced is not attributable to any other dental diseases or conditions that can produce similar symptoms, e.g., dental caries.
If our patients suffer from DHS, the affected teeth can be sensitive to slight cold or heat, acidic or sweet drinks and foods, when gently touched, and sometimes when cold air is breathed in. The resulting short sharp pain can affect patients' lives during activities such as speaking, eating, drinking and brushing their teeth. It is important to address DHS. It can not only affect a patient's activities and quality of life, longer-term it can also affect the patient's emotional and psychological well-being.
Since episodes of DHS might be a common occurrence for our patients, they may be less likely to disclose their symptoms with the belief that these are normal. We must therefore ask questions to prompt our patients to fully describe their issues. We can ask whether they have sensitive teeth, what triggers the pain - for instance, do they suffer from pain when eating or drinking cold or hot foods or drinks, can they describe the pain, can they localize pain to any specific teeth or areas? Other questions to ask prior to performing a clinical examination include:
- Post-op sensitivity following tooth preparation - have they had any fillings or other restorative work recently?
- Have they received treatment for periodontal (gum) disease?
- Post-op whitening sensitivity - have they recently whitened their teeth?
- Did they crunch down on something that caused pain?
- Trauma - have they fallen and hit their teeth or had any injury to the face that may have affected their teeth?
- Do they grind their teeth?
- Do they suffer from GERD? Or bulemia?
As well as a good patient history, a thorough clinical examination is necessary to differentiate DHS from the other potential causes for the pain, such as dental caries, lost or defective restorations, cracked teeth, and trauma. It is also necessary to identify exposed dentin. Clinical signs suggesting DHS include:
- Exposed dentin
- Gingival recession
- Areas affected by dental erosion
- Facets or shallow grooves at the gingival margin
- Areas with abrasion and/or attrition
We should ensure we document any of these clinical signs and monitor them.
How can we manage DHS?
There are many options for managing DHS that we can offer patients who suffer from DHS. These can include:
- Use of a desensitizing toothpastes, such as Colgate Sensitive Toothpaste which contains potassium nitrate, is proven to relieve DHS and provides long-lasting relief with continued use.
- Application in-office and at home of Colgate Anywhere Anytime Sensitivity Relief Serum for rapid relief
- In-office application of 5% sodium fluoride varnish, such as Colgate PreviDent Varnish
In a number of cases, bonded resins are applied, or restorative interventions or coverage with gingival surgery are provided.
It is vital for students to ask the right questions when assessing our patients in order to then diagnose and treat common problems such as DHS. Managing DHS can actually be straight forward with in-office and home use products, and can really improve the quality of life of our patients.
Was this article helpful?
If you’d like a response, Contact Us.